
Median temperature of the perfusate was 32 ☌. Bicaval cannulation was performed and cardioplegic arrest was done by antegrade cold crystalloid cardioplegia. Surgical repair was performed by consultant level cardiac surgeons through median sternotomy. Approval of the institutional review board was obtained before data collection and the need for patients’ consents was waived due to the retrospective nature of the study. A total of 322 patients were included in the study. Moreover patients with serious postoperative arrhythmia other than JET ( n = 17) and patients with missing postoperative JET diagnosis criteria from the medical records ( n = 23) were excluded. We excluded patients older than 2 years ( n = 231) and patients with rhythm disturbances or heart block preoperative ( n = 16). A total of 609 patients underwent surgical TOF repair between January 2003 and December 2017. This is a retrospective cohort study performed at King Faisal Specialized Hospital and Research Centre in Jeddah, Saudi Arabia. The objectives of this study were to characterize patients with JET, identify its predictors and subsequent complications and the effect of various treatment strategies on the outcomes in selected TOF patients undergoing total repair before 2 years of age. Although many studies were concerned with postoperative arrhythmia, little have focused on JET following total TOF repair in infants. Generalization of preoperative prophylaxis for arrhythmia in all patients undergoing surgery for congenital heart defects is non-practical and preoperative identification of high risk patients is essential.

Recently, the effect of several pharmacologic agents on reducing postoperative JET was evaluated.
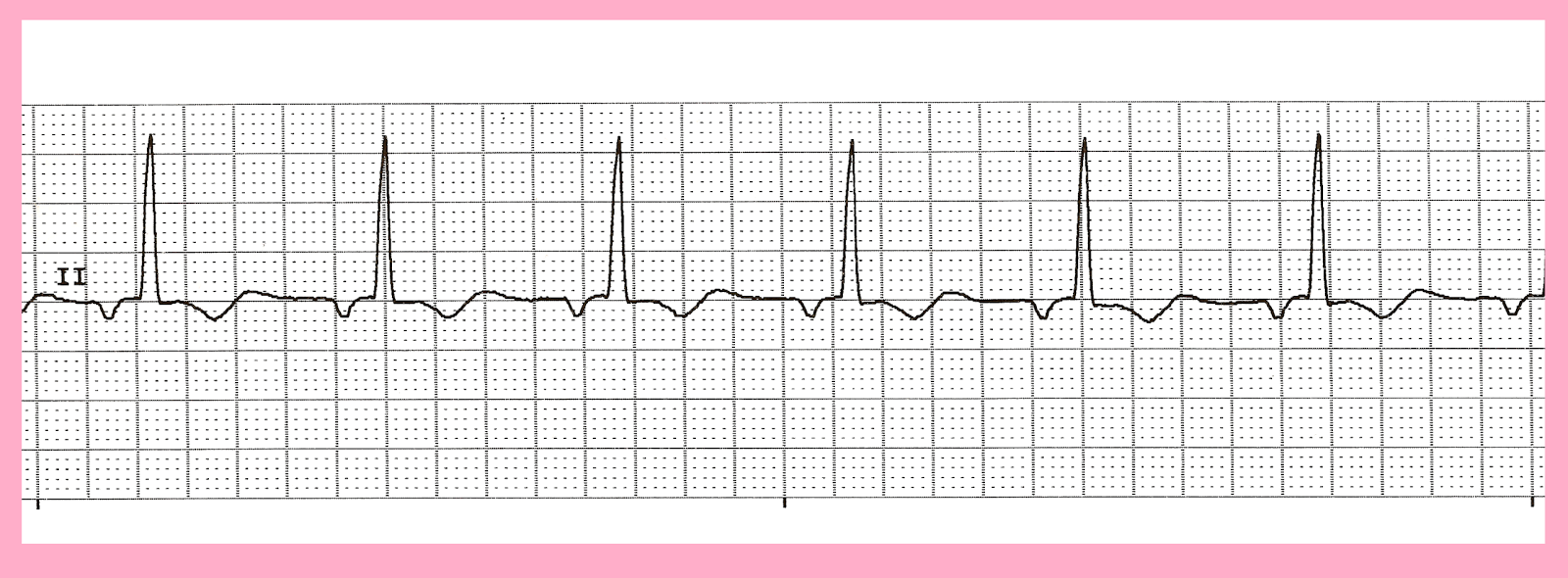
Several treatment strategies ranging from pharmacologic agents to atrial cardiac pacing are used sequentially to lower the ventricular rate and re-establish atrioventricular synchrony. Incidence of JET is higher when the intervention is close to the atrioventricular node and bundle of Hiss as in tetralogy of Fallot (TOF) and complete atrioventricular canal (AVC) repair. The incidence of JET following congenital cardiac surgery varies widely in literature which can be attributed to the different diagnostic criteria and the great variability in the patients’ characteristics among the published studies. Postoperative junctional ectopic tachycardia (JET) is a potential life-threatening arrhythmia occurring after congenital cardiac surgery. Patients with preoperative risk factors could benefit from preoperative arrhythmia prophylaxis and aggressive management of postoperative electrolyte disturbance is essential. Preoperative B-blockers significantly reduced JET. Timing of JET onset didn’t affect ICU ( p = 0.43) or hospital stay ( p = 0.14) however, long duration of JET increased ICU and hospital stay ( p = 0.02 and 0.009 respectively). Median duration of JET was 30.5 h and 5 patients had recurrent JET episode. Ventricular pacing was required in 4 patients (5.2%). Amiodarone was used in 31.25% ( n = 30) of patients and its use was associated with longer ICU stay ( p = 0.017). JET resolved in 39.5% ( n = 38) of patients responding to conventional measures. JET didn’t affect the duration of mechanical ventilation nor hospital stay ( p = 0.12 and 0.2 respectively) but prolonged the ICU stay ( p = 0.011). Independent predictors of JET were younger age, higher preoperative heart rate, cyanotic spells, non-use of B-blockers and low Mg and Ca ( p = 0.011, 0.018, 0.024, 0.001, 0.004 and 0.001 respectively). JET patients were younger and had higher preoperative heart rate. 29.8% of the patients ( n = 96) had postoperative JET. We excluded patients above 2 years and patients with preoperative arrhythmia. Methodsįrom 2003 to 2017, 609 patients had Tetralogy of Fallot repair, 322 were included in our study. Arrhythmia prophylaxis is not feasible for all pediatric cardiac surgery patients and identification of high risk patients is required. Junctional ectopic tachycardia is a serious arrhythmia that frequently occurs after tetralogy of Fallot repair.


 0 kommentar(er)
0 kommentar(er)
